
Scientific background
We developed our GAL+ Multivitaminl® product in light of the latest research, bearing in mind the need for it to be natural and life-like, that it should contain every vitamin, mineral and trace element in ideal form, amount and proportion, not deviating from how we would obtain all these following a steady, nutrient-rich, varied diet. Where beneficial, the vitamins and minerals partly come from organically farmed medical herbs and spice extracts. In terms of amounts, we deemed it important all along that the daily intake must contain the dosage found effective but on no account should it exceed realistic amounts, i.e. the amount that could be covered by nutrition. In addition it’s extremely important that nothing that doesn’t belong there is underfoot. No trace of such thing will you find in our product.
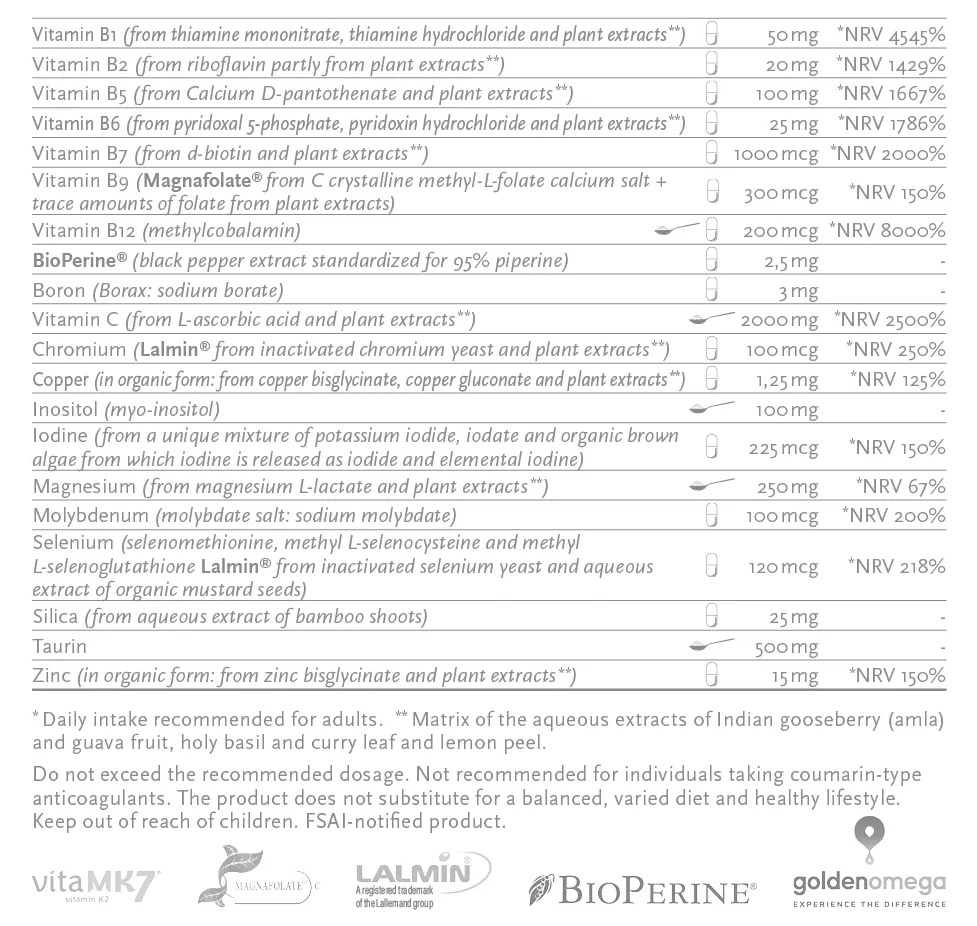
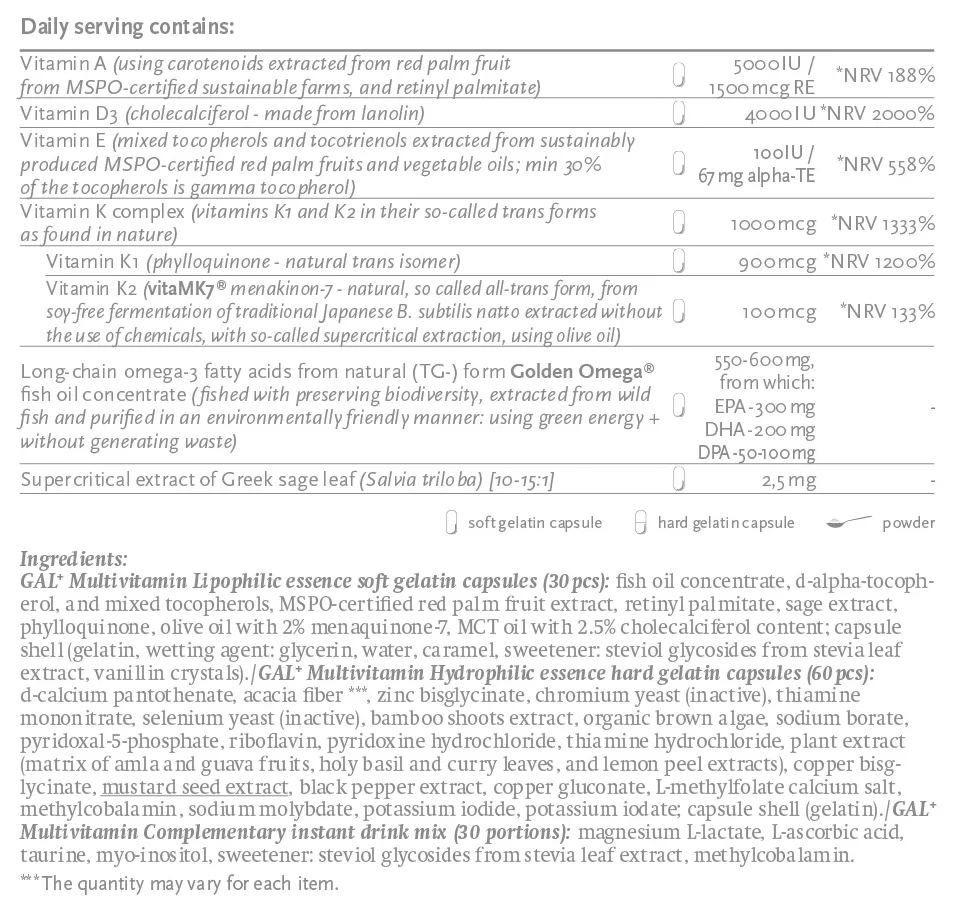
Although all the active ingredient forms used have excellent absorption in the first place we boosted it with Bioperine® black pepper extract. We were also careful not to mix water-soluble and fat-soluble ingredients so they can be present separately, in a way that guarantees ideal absorption and stability.
Some of the water-soluble (hydrophilic) ingredients are contained in hard gelatin capsules together with the matrix of the plant extracts mentioned earlier. Those active ingredients which are best taken evenly distributed throughout the day are presented as a complementary drink powder that can be sipped away during the day.
Fat-soluble (lipophilic) ingredients are contained in soft gelatin capsules dissolved in GoldenOmega® fish oil concentrate, stabilized with natural tocopherols/tocotrienols and Greek sage extract.
Besides the usual multivitamin components, it contains large quantities of magnesium, taurine, silicon obtained from bamboo shoots, vitamins K1 and K2 and long-chain omega-3 fatty acids in natural (TG) form (EPA, DPA, DHA), produced from small wild fish caught and processed in an environmentally friendly way.
It contains vitamin B9 in active methyl folate form that can also be found in the body. We use it as its most stable, C crystal structure calcium salt, Magnafolate®, which is even more stable than methyl folate’s glucosamine salt.
Our GAL and GAL+ Multivitamin, as well as GAL and GAL+ Prenatal Multivitamin products, were developed in the light of the latest research while keeping naturalness and lifelikeness in mind. This means that the product contains all vitamins, minerals and trace elements in the same ideal form, quantity and ratio as one would consume in the course of constant, diverse and nutritious food intake.
It may sound surprising, but it is at least equally important, what it does NOT contain...
This was in fact one of our motives to create a new multivitamin, as we found out that there wasn’t a single one without at least one ingredient - in the country or in the EU - which the author of this article would not put in his mouth, even if he would be paid for it... (this mainly does not apply to the excipients, but to the wrong forms or exaggerated quantities of the agents).
Here I would not go into the details of vitamins (e.g. vitamins D, E and K), minerals (e.g. magnesium) and dietary supplements (e.g. fish oil) introduced many times in many places, and would not thoroughly address what they contain in what quantities and forms and why. I would, in turn, highlight a few ingredients I feel it is important to explain, like why they contain, for example, iodine, choline and vitamin A, why they contain methyl folate instead of folic acid, and why they do not contain iron.
Let’s see the details.
Iodine (and Selenium)
Iodine is not only important for the thyroid gland. Among others, the brain, ovaries, women’s breasts and testicles use more iodine than the thyroid gland, provided that the iodine reserves of the organism are sufficient, in the ideal case that is. It is said that many physicians still consider iodine only in connection with the thyroid gland, and often recommend fully avoiding iodine (even food with iodine content) to their patients with thyroid gland issues or to patients, whose thyroid gland has been removed. The reason many physicians make this recommendation is that certain analysis suggests that iodine supplementation and/or high iodine intake might increase the risk of thyroid gland problems, or in case of those suffering from autoimmune thyroid gland disease - not often though - iodine supplementation may temporarily result in slight deterioration of the test results. Other examinations found just the opposite. i.e. that high iodine intake does not increase, but actually and explicitly decreases the risk of thyroid gland diseases, and that additional iodine intake did not deteriorate the values of patients with autoimmune thyroid gland disease, either. So the analyses in the field of iodine supplementation are contradictory. There is full consensus, however, that adequate intake of selenium does reduce the risk of thyroid gland diseases, improves the existing thyroid gland problems, and protects from a potential adverse effect of iodine. The analyses summarily suggest that if there is no lack of selenium, then iodine is not harmful, but is useful. The iodine level of the thyroid gland of patients suffering from autoimmune thyroid gland disease is always a lot lower than the iodine level of the thyroid gland of healthy people. And the worse one’s condition is, the lower the iodine content of the thyroid gland would be. The iodine intake of Japanese people - who consume the most iodine in the world - is well above 1,000 mcg per day (typically between 1,200 and 13,000 mcg, but higher volumes aren’t rare, either). Still, many diseases of the thyroid gland are rarer in their case, and even Hashimoto is not more frequent. In turn, their selenium intake is also high.
One of the main factors causing thyroid gland problems is always the lack of iodine, and so recommending an iodine-deficient diet will cause certain disasters over time (it’s another problem that with taking medication containing thyroid gland hormone, values can be better without iodine, but the lack of iodine only increases the cause of the problem).
So, should we or should we not take it in case of a thyroid gland problem? And how much?
The ideal solution is to take the most iodine we can without causing deterioration of the laboratory values. Before taking any iodine it is important to make sure that our selenium level is in order (and preferably our magnesium and vitamin C levels, as well). If we do not often consume food rich in selenium (liver, all kinds of saltwater fish/seafood and mustard are good sources of selenium), then we should take 200 mcg of selenium for 2 to 4 weeks, e.g. in form of selenium yeast. And we should also take at least 2000 mg of vitamin C each day (well distributed throughout the day) + well-absorbing magnesium compound (e.g. in form of Mg-lactate/biscyglinate/ascorbate/orotate) equal to 200 to 400 mg elementary magnesium. After this, we can safely take 225 mcg of iodine, which quantity can even be increased later. After starting to take iodine, selenium intake can be reduced to 100 to 120 mcg (there is typically 50 to 100 mcg of it even in food not rich in selenium). It is important that everyone suffering from a disease of the thyroid gland - or people whose thyroid gland has been removed - should consume at least 225 mcg of iodine each day. In case, if - despite optimizing selenium level - any of the values become worse as a result of taking iodine (the chances for that are rather slim), then stopping gluten intake will probably solve the problem. If it would not, then avoiding legumes, food containing Neu5gc (mammals), or food belonging to the potato family (i.e. auto-immune protocol nutrition, AIP) will surely solve the problem.
Iodine for pregnant women?
It is especially important that even a very slight iodine deficit would reduce the expected IQ level of the child by 8 to 16 points. Severe iodine deficit could even lead to cretinism (Congenital iodine-deficiency syndrome). In addition, the child’s ADHD risk is further increased, if the mother suffers from iodine deficit during pregnancy and/or breastfeeding. Still, many doctors prohibit taking iodine even for pregnant women suffering from thyroid gland disease. In this case, too, the selenium level has to be optimized first, and only then the iodine supplementation can be started.
That is why we added 225 mcg iodine to our GAL and GAL+ Babaváró, as well as to GAL and GAL+ Multivitamin products, because - provided that the selenium level is adequate - it very rarely causes problems, even in case of severe autoimmune thyroid gland disease, but on a long term, it is sufficient to ensure optimal iodine level.
The selenium level is 120 mcg instead of 200 mcg, because taking 200 mcg in the long run (let alone the selenium contained in the food we eat) may result in an excessive selenium level that is beyond the optimal, and may also cause problems. (120 mcg of selenium of the forms we use is abundantly enough, as it originates partly from methyl-l-selenocysteine and methyl-l-selenoglutation; these are more active forms, with higher tolerance and better absorption).
For those who want to go deeper into the topic of iodine, I recommend the books of Dr David Brownstein, Dr Jeffrey Dach, Dr Guy E. Abraham, the works and research of Dr Jorge Flechas, as well as the book The Iodine Crisis recently released in Hungarian, too.
Furthermore:
https://jeffreydachmd.com/hashimotos-selenium-and-iodine-part-two/
Dr. Jorge Flechas: AutoimmuneThyroiditis and IodineTherapy. Journal of RestorativeMedicine. 2013.
https://www.bmj.com/content/352/bmj.i941/rr-2
Vitamin A
Why the supplementation of vitamin A is important and dangerous at the same time, and can it be optimized?
Vitamin A (retinol) contained in our body can originate from two sources:
- carotenoids (mainly alfa and beta carotene) contained in our food (mainly in vegetables) are transformed into retinol by the organism.
- Food of animal origin already contains vitamin A (retinol)
Both deficiency and surplus of vitamin A are harmful. Its surplus causes a relative deficiency of vitamin d3 on the receptor level, and so it is harmful (due to which D3 reduces its toxicity). On the other hand, the body transforms carotenoids into retinol only in the required quantity, so no overdosing is possible in this case (although a research test found the supplementation of both vitamin A and beta-carotene harmful; taking them increased the risk of lung cancer for smokers. But in that research synthetic beta carotene was used, and carotenoids are never present in food only in form of beta carotene, there is always at least alfa carotene present, too, so it is not lifelike, and the same problem exists, as in case of another test, where the supplementation of vitamin E was found harmful... it turned out that vitamin E was only present there as alfa-tocopherol, although gamma-tocopherol, for example, is much more efficient in many ways, and tocopherols are always present together in food, so taking vitamin E as only alfa tocopherol is harmful, even if it comes from natural sources, as it distorts the natural tocopherols ratios of the tissue. We take something that is good, but by doing so we reduce something that is even better - so the net impact is negative.)
Getting back to vitamin A... If taken in form of mixed carotenes, there is no risk, you can’t take too much of it, because the body produces only as much retinol as it requires. In form of retinol, however, it can easily overdose. So it would seem obvious that we should take it in the form of mixed carotenoids... But without zinc, we cannot transform it in a necessary manner. Well, let’s take zinc, as well, no problem. All right, but some people - for genetic reasons - are not able to produce from carotenoids a sufficient quantity of retinol, even in case of ingesting the appropriate quantity of zinc. To them, vitamin A is important also in form of retinol!
The liver is practically the only food with relevant vitamin A (retinol) content. 100g liver contains approximately 20 thousand NE vitamin A (between 10 and 80 thousand NE). Our body requires 2 to 8 thousand NE retinol on daily basis. Both lower and higher quantity is harmful. This means that eating liver at least once a week will eliminate the risk of vitamin A deficiency, but eating 2 to 3 times a week plus taking 5000 NE retinol per day (e.g. with multivitamins) could be too much... would be optimal for those not eating liver.
Because of the above Multis and Babavárós contain 5000 NE so-called vitamin A equivalent, half of which, 2500 NE comes from mixed carotenoids, from RSPO-qualified (i.e. orangutan-friendly) carotenoids extracted from red palm fruit (mainly alfa, beta and gamma carotenoids, but also other carotenoids and lycopene, although it is not indicated, because it is not transformed into vitamin A by the organism). The other half (2500 NE) comes from retinol. This way those, who do not eat liver, and are unable to transform carotenoids contained in vegetables into retinol, either, still get a sufficient quantity of retinol, while the +2500 NE retinol per day would not be too much for those who eat much liver. The zinc content of the product is abundant enough to maximize the conversion of retinol from carotenoids, where this is the bottleneck.
Methyl folate - folic acid
Vitamin B9 is known as folic acid. It should be noted that folic acid does not occur in nature, in food products, or in our bodies. Folic acid is a completely foreign substance. So-called folates occur in nature (in food products of vegetable - but also animal - origin), and/or - since the ingested food folates are transformed into methyl folates in animals (and in people, as well), food products of animal origin - besides folates - also contain methyl folate, as well. Methyl folate is the active formula, so the only thing that matters is how much methyl folate is contained in our bodies.
Folic acid is used in various dietary supplements, medications to enrich food products, in cereals, etc., because folate is unstable, so it can only be contained in fresh food.
Folate could be extracted and put in capsules, but by the time of reaching the user, it would decompose and have no effect. Folic on the other hand is a stable form, and with the help of enzymes, in the ideal case, it is transformed into folate, and then into methyl folate. The problem is that nearly 90 per cent of the people have problems with the utilization of folic acid, while 60 per cent have significant problems, these are people with the so-called MTHFR gene variant. Approximately 10 per cent of people are able to transform 100 per cent of the folic acid into folate and then the folate into methyl folate, whereas 60 per cent of people are hardly capable of transforming it, or are not capable at all. They may have folate deficiency even in the case if they ingest a sufficient quantity of folate (e.g. by eating plenty of vegetables) because only a small part of the active form of methyl folate is transformed. On the other hand, folate cannot do any harm, the worst it can do is be useless if a sufficient quantity of it is not transformed into the active methyl folate. On the other hand, it may even be harmful, if we take medication/dietary supplements containing folic acid, or consume food enriched with folic acid, as at that point a large part of the folic acid is not transformed into folate, either, and such unmodified folic acid starts accumulating in our tissues and blood. This means that a foreign substance that has nothing to do with our body, starts accumulating... This is a warning sign in itself, but a correlation has been found between the level of UMFA (unmodified folic acid) and various diseases, such as colon cancer. Research on the subject has been started only recently, and who knows what else is to turn out...
That is why it is vital for most people to avoid all products that contain B9 vitamins in form of folic acid. The most efficient, active and natural form of B9 is methyl folate (both its calcic salt and glucosamine salt is adequate), but folic acid (e.g. calcium folinate) is also sufficient for most people, except for those with homozygous MTHFR mutation (e.g. 10 per cent of the population).
Since 200 mcg of the active methyl folate form is sufficient for anyone (even during pregnancy), but more of it would not cause any trouble, either, so our products contain 200 to 600 mcg of it (and none of the folic acid).
Iron
Iron has a strong oxidative, destructive impact in our body for all cells, so it is important to keep our free iron level as low as possible. At the same time, iron plays an indispensable role in numerous body functions, so its lack is also a problem.
For most pathogens, too, iron is an important nutrient, so iron supplementation and the high iron level in itself boost the proliferation of pathogens, and so it makes any chronic or acute infection even more severe. That is why in the ideal cases our cells store iron bound to ferritin, especially in case of infection, because for most pathogens iron is inaccessible when bound to ferritin. This is the main strategy of the body to deprive pathogens of iron, and so to protect itself against infections. Ferritin plays an important role also in the transportation of iron, as well as in regulating our free iron level. If a part of our body needs more iron (e.g. for the immune cells to produce peroxide, which it uses against harmful cells/pathogens), then ferritin transports the iron there, whereas in turn, if the iron level in our blood gets too high, then ferritin stores the surplus, thus reducing it to the ideally low level.
Iron supplementation and frequent consumption of food rich in iron is also a problem because it has an adverse impact on the intestinal flora and on the intestinal system in general. So the first step, where iron can do harm, is our digestive system. From there - reaching the bloodstream - it gets to all of our cells, and in the course of its oxidation causes harm to blood ingredients and the cells by producing harmful substances. It also boosts the number of pathogens (mainly those inside the cell, but also those outsides of it). On the other hand, if our ferritin level is sufficient, and the iron intake is not too high, either, then these harmful impacts cease or at least reduces. Ferritin, on the other hand, does not eliminate the harmful impact on the intestinal system, so it is still important to keep our iron intake low (in the presence of sufficient ferritin, little iron is sufficient, because it boosts its absorption and transportation to the right location).
During pregnancy, it is especially important to keep our iron level low, whereas at the same time, our iron reserves are at an optimal level, as well. So settling the iron level is better, if not done through iron supplementation, because the latter is harmful to the fetus, as well. In research conducted in Italy in 2014, nearly 300 pregnant women with iron deficiency or anaemia were divided into two groups. 156 mothers in one group received 2 x 100mg lactoferrin per day, whereas the remaining 139 mothers were given daily 560 mg sulfate supplement. In the group taking lactoferrin (a group with no iron) all test results on iron (haemoglobin, iron, ferritin, etc.) significantly improved, i.e. iron deficiency anaemia were completely eliminated, whereas the same values in the other group taking iron did not improve, but further deteriorated instead. In the group of mothers taking lactoferrin only, no side effects were observed, and their values indicating body-wide inflammation also improved, whereas, in the group of mothers with iron deficiency taking iron, the inflammation level further deteriorated, moreover, iron supplementation caused detectable side effects to more than 16 per cent of them. Most surprising during the project, however, was that in case of mothers not taking iron, only lactoferrin no abortion occurred, and all babies were born healthy, whereas in the group of mothers taking iron 5 abortions occurred, which is 4 per cent of all cases!
So, if possible, iron should never be supplemented. Of course, if we have iron deficiency, then it is important to optimize the iron level of our body, but it is seldom feasible with iron supplementation only. In case of pregnancy, intestinal problems, or chronic or acute inflammation it is particularly worth optimizing our iron level without iron supplementation.
So what should we do against an iron deficiency?
We should definitely have also our ferritin level measured. In an ideal case, during pregnancy, it should be kept between 50 and 75 ng/ml (according to other opinions: between 20 and 75 ng/ml). Ferritin level increases in case of acute/chronic inflammations, infections and often in case of obesity/metabolic syndrome, however, low ferritin level always means low iron status, and/or that only a small part of the iron present in our body is in its ideal “storage location”, - in ferritin, which means that in cases like this, the high or normal iron level is extremely harmful. Ideally, our iron level is low-medium, whereas ferritin, transferrin and haemoglobin levels are normal.
Although keeping the ferritin levels low may have its advantages in extending life expectancy (at approximately 20 ng/ml), still it is worth aiming at values around 50 ng/ml (between 50 and 75), especially in the case of pregnancy. If we are in this value range, then our iron level doesn’t matter, it’s ok, even good if it is low. In most cases, lactoferrin quickly increases our iron level, as was demonstrated in the test referred to above, and reduces harmful effects of iron (deprives pathogens of iron, helps to transport the iron to the healthy cells, increases iron intake by the cells, whereas helps to store the surplus iron in form of ferritin).
Vitamin C also helps in increasing the ferritin level. On the other hand, coffee, chocolate, tea, seeds, legumes, whole-grain products, and food products containing other phytic acids and catechins reduce both iron and ferritin levels.
So we have to deal with an iron deficiency if our ferritin level is low (below 50 ng/ml). In this case, first, we should try and settle our ferritin level by taking lactoferrin and vitamin C, and by avoiding agents reducing iron/ferritin levels. As a daily minimum, 2 x 100mg lactoferrin (it can safely be more, even 2x30mg) + daily minimum of 2000mg vitamin C (it can even be 10 thousand mg, but for the sake of proper absorption it is important not to take more than 1000mg at a time), and/or reduction of consuming tea/coffee/legumes/seeds/wholegrain “brown things”.
If this does not settle our ferritin level (and our iron status with it), then it is best to start eating more liver (e.g. 3 times a week) and/or more red meat or other food (preferably of animal origin) with iron content in addition to the intervention recommended above (it is recommended to take vitamin C together with food containing iron, especially if the source of the iron is of plant origin) This should work, but if somebody is not willing to eat liver more often, and his/ferritin does not go up to 50bg/ml, i.e. as a last resort, iron supplementation with medication or dietary supplements can be considered (especially, if the ferritin level is below even 30ng/ml).
Warnings
KEEP OUT OF REACH OF CHILDREN. DO NOT EXCEED RECOMMENDED DOSE.
If you are undergoing treatment for a medical condition or if you are pregnant or lactating, please consult your medical practitioner before introducing supplementary foods to your normal routine. The dietary supplement should not be used as a substitute for a varied and balanced diet or a healthy lifestyle. Store tightly closed in a cool and dry place.
- Allergen-free
- Glutenfree
- Egg-free
- Soy allergen-free
- Dairy and lactose-free
- Free of sulfur dioxide
- Sugar-free
- GMO-free
- Vegetarian
- Vegan
- RSPO / Orangutan friendly
- FSC paper material (CO31340)
- Packaging from carbon-neutral production
- 100% recyclable packaging
Green: The product has the described property
Red: The product does not have the described property

